Clostridioides difficile infection (CDI) linked to 220,000 hospitalized patients
Clostridioides difficile (CD) is a gram-positive bacillus commonly found in soil that can cause antibiotic-associated diarrhea. Clostridioides difficile infection (CDI) is linked to 220,000 cases in hospitalized patients and is responsible for about 13,000 deaths per year in the United States. As a result, CDI creates over $4.8 billion in medical expenses per year in the United States.
Affected individuals are typically younger, with an average age of 50 years.
A recent review gathered evidence that patients using cannabis regularly had lower odds of being diagnosed with CDI.
Clostridioides difficile (CD) causes cell death
Clostridioides difficile is resistant to multiple antibiotics, and colonization with CD most commonly occurs following antibiotic treatment for other diseases; the resulting post-antibiotic harm to the intestinal flora promotes CDI.
Its spores are easily transmitted through the fecal-oral route and are challenging to eradicate. CD produces toxins that disrupt enterocyte intercellular junctions, causing cell death and promoting transmural invasion.
Typical symptoms include diarrhea followed by fever and abdominal pain. Severe CDI or fulminant CDI may be life-threatening. Once the diagnosis is confirmed, measures to prevent transmissions like isolation and strict adherence to hygiene measures must be implemented.
With this work, researchers Adeyinka Charles Adejumo and Terence Ndonyi Bukong illuminated the impact of cannabis use on CDI incidence amongst hospitalized individuals.

Cannabidiol (CBD) effects on disorders, dysfunctions, and pathologies
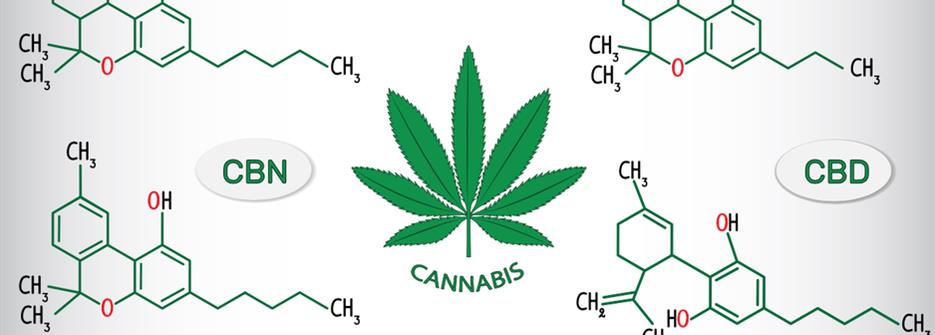
Cannabinoids, considered to have antibacterial attributes, are most well-known as one of the more than 500 components in the plant cannabis. As a non-psychoactive component derived from the cannabis plant (Cannabis sativa), cannabidiol (CBD) demonstrated positive effects on several psychiatric disorders, metabolic dysfunctions, and malignant pathologies.
Basic science research confirmed antibiotic properties of cannabinoids against staphylococcus aureus and protection from endotoxin-induced septic shock syndrome, as well as neurological damage from streptococcal pneumonia meningitis.
In-vitro studies showed inhibition of CD conceivably through a variety of effects. Firstly, by promoting enhanced gut integrity and homeostasis. Secondly, by modulation of the intestinal microbiome composition. Evidence indicates that by shifting the microbiome balance in favor of lower firmicutes and higher bacteroidetes, cannabinoids have gut protective characteristics. Thirdly, cannabinoids were able to suppress intestinal inflammation in murine models. Lastly, cannabinoids proved to impede the toxicity of clostridium bacteria in in-vitro cultures.
Nevertheless, in contrast, tetrahydrocannabinol (THC), a pharmacologically active component of cannabis, suppresses stomach acid secretion; decreased gastric acidity is sought to be an independent risk factor for CDI.
Cannabis is related to decreased CDI
This publication, Cannabis use and risk of Clostridioides difficile infection: Analysis of 59,824 hospitalizations, highlights that cannabis, in an increasing dosage, is related to decreased incidence of CDI. Still, the broader mechanism of cannabis on this disease remains ill-defined.
Further research into the mechanism and relationship underlying the antibiotic properties of cannabis might be fruitful. More extensive prospective cohort studies are needed to translate preclinical findings on cannabinoids and CDI to clinical research.